Laura Heltz, Executive Director & U.S. Army Veteran
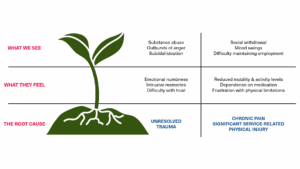
For more than a decade, I’ve been working with veterans who struggle with substance abuse. I’ve seen veterans at every stage of recovery – some of whom were able to overcome their addiction; others who relapsed; and, tragically, some who overdosed. In too many of these cases, this all could have been avoided if not for their reliance on prescription opioids. These brave servicemembers stood up for our country and freedoms only to be knocked down by addiction to medication that is supposed to help them manage chronic and post-surgical pain. This is an epidemic that is unfair to the people who served our country.
Veterans and Opioid Use by the Numbers
I’ve been doing advocacy for with a fantastic organization called “Voices for Non-Opioid Choices.” They are a “nonpartisan coalition dedicated to preventing opioid addiction before it starts by increasing patient and provider access to non-opioid therapies and approaches to manage acute pain.” They report that:
Nearly half of combat-wounded veterans report misuse of prescription opioids.
Drug overdose mortality rates among veterans increased by 53% from 2010 – 2019.
The healthcare costs of prescription painkiller abuse among service members is roughly $1 billion a year.
They go on to say that “Acute pain patients often receive powerful, addictive medications to manage their pain. The surgical setting, in particular, has become a potential path to long-term opioid abuse in America.”
In July 2022, the Substance Abuse and Mental Health Services Administration (SAMHSA) released its 2020 National Survey on Drug Use and Health: Veteran Adults. This report found that in 2020:
490,000 veterans aged 18+ reported prescription opioid misuse.
53,000 veterans aged 18+ reported prescription opioid misuse and heroin use (heroine is a chemically similar drug to opioids, and prescription opioid use can be a steppingstone to other drugs).
Misue of prescription pain relievers is much more common than heroin use.
And these are just the veterans who chose to report the misuse. The number of veterans misusing prescription opioids and those using both the prescription and heroin/other drugs is undoubtedly higher than this.
How We’re Advocating for Veterans
On April 17th, Veterans Outreach Center and 79 other organizations signed a letter written by Voices for Non-Opioid Choices to the U.S. Department of Veterans Affairs urging them to update their coverage policy to include non-opioids in their formulary. The formulary is a list of medications and related information that guides prescribing practices, based on the judgment of healthcare professionals. You can read the full letter here, but this paragraph is of particular importance:
“Unfortunately, the VA National Formulary (“VANF”) does not include several FDA-approved, safe, and effective non-opioid analgesic products, meaning VA patients have little choice in managing their acute pain symptoms. As a result, the policy embraced by the VANF unnecessarily exposes our nation’s veterans to opioid-based analgesic products. This decision is putting their lives in jeopardy.”
Our veterans need to be set up for success after their military service, and that includes access to non-addictive, non-opioid prescriptions.

I’ve also spent time on Capitol Hill in Washington, D.C., meeting with House and Senate
members/staffers to advocate for H.R.10396 – NOPAIN for Veterans Act. Introduced into the house on December 12th, 2024, this bill does exactly what the letter we signed asked the VA to do: “To amend title 38, United States Code, to ensure that the Secretary of Veterans Affairs furnishes certain non-opioid pain medications to veterans, and for other purposes.”
As I said at the beginning – I’ve been working with veterans who have been dealing with
substance abuse for more than a decade. It feels good to start looking at ways to get upstream of this problem instead of always reacting to it after the fact. The absolute s
urest way to reduce opioid addiction is to ELIMINATE exposure in the first place. And that starts in the healthcare setting.