Jeff Klein, Wellness Programs Manager
As access to mental health research and resources has grown over the years, a number of studies have been conducted to identify the benefits of mindfulness. A quick look at Google Trends shows that interest in web searches for “mindfulness” has increased significantly over the past 10 years. Interestingly, searches for “mindfulness” reached 100 (peak popularity) in April 2020. Presumably, this is due to people searching for ways to cope with the stress of the pandemic. The chart below shows the growth of mindfulness Google searches from 2004 (ranking 10) through June 2025 (ranking 64).
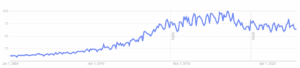
A note on the “Interest over time” rankings from Google: “Numbers represent search interest relative to the highest point on the chart for the given region and time. A value of 100 is the peak popularity for the term. A value of 50 means that the term is half as popular. A score of 0 means there was not enough data for this term.”
As interest in mindfulness surged, researchers began exploring the benefits specifically for veterans with post-traumatic stress disorder (PTSD) and found some positive results.
What is Mindfulness?
The American Psychological Association defines mindfulness as “awareness of one’s internal state and surroundings. The concept has been applied to various therapeutic interventions – for example, mindfulness-based cognitive behavior therapy, mindfulness-based stress reduction, and mindfulness meditation – to help people avoid destructive or automatic habits and responses by learning to observe their thoughts, emotions, and other present-moment experiences without judging or reacting to them.”
In short, it’s the practice of being aware of your mind, body, and feelings in the present moment to create feelings of calm.
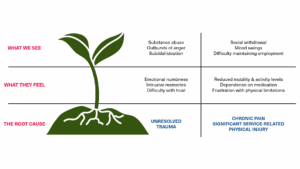
The Mayo Clinic states that “spending too much time planning, problem-solving, daydreaming, or thinking negative or random thoughts can be draining and make you more likely to experience stress, anxiety, and symptoms of depression.” For veterans with PTSD or other mental health challenges, stress, anxiety, and symptoms of depression may stem from experiences during their military service.
Mindfulness and PTSD
1. Mindfulness-Based Processes of Healing for Veterans with Post-Traumatic Stress Disorder
A research paper from the National Library of Medicine titled Mindfulness-Based Processes of Healing for Veterans with Post-Traumatic Stress Disorder conducted a study using in-depth interviews with 15 veterans after attending multiple mindfulness sessions. All veterans in the study had a positive PTSD diagnosis, and the results were promising:
Veterans identified six core areas that the mindfulness sessions helped with:
Dealing with the Past: Helped deal with memories differently and created interest/curiosity in how they got to where they are. They also opened the possibility of revisiting locked away memories and allowed them to come to a better understanding of themselves. One participant described finding “that peace and forgiveness, and I can start to relieve some of that guilt.”
Staying in the Present: Participants reported feeling less caught up in thoughts about past or future events as a key skill, offering protection from distressing thoughts about the past.
Acceptance of Adversity: Participants said the mindfulness activities helped them accept their current reality, even when it was challenging, and allowed them to see pain in a different light.
Breathing Through Stress: This gave the participants an alternative to stressful situations and allowed them a moment to work through their stress first before reacting.
Relaxation: Helped participants feel more relaxed and physically better. Some said it helped them fall asleep and described a “warmness” in the body and a “cleansing feeling.”
Openness to Self: The mindfulness activities helped the participants become kinder to themselves, which enhanced their relationships. Some described the group structure of the activities and instruction as helping them become more open to others.
2. VA Management Brief No. 88: Evidence Map of Mindfulness
A Management Brief from the Department of Veterans Affairs (VA) reported that “the most consistent beneficial effect for various mindfulness interventions was reported for depression. Published meta-analyses of MBSR also indicated beneficial effects compared to passive control (e.g., no intervention) on overall health and psychological outcomes and for chronic illness. In addition, reviews indicated positive effects of Mindfulness-based Cognitive Therapy (MBCT) for mental illness and of various mindfulness interventions for somatization disorders.”
In short, mindfulness activities showed to help with symptoms of depression, overall health, mental illness, and chronic illness. It also helped with “somatization,” or the conversion of a mental state, such as depression or anxiety, into physical symptoms.
3. VA Researcher Exploring Meditation as a Therapy for PTSD
An article from the VA Office of Research & Development, VA Researcher Exploring Meditation as a Therapy for PTSD, reported that Dr. Ariel Lang, Director of the Center of Excellence for Stress and Mental Health at the VA San Diego Healthcare System and Clinical Phycologist and Professor at University of California San Diego found a connection between mindfulness/meditation and relief from PTSD symptoms.
“You can think of PTSD in some way as an attention disorder,” Dr. Lang said. “What happens when someone has a flashback or an unwanted memory is their attention is diverted to someplace else, someplace they don’t want to think about right now. If you think about it that way, managing PTSD is about keeping your attention where you want it to be. One thing that meditation does – and this is certainly true of mindfulness meditation – is help to train attention.
“PTSD is also a disorder of arousal, so you get the jumpiness, the physical sensations, the panic-like symptoms. It looks like meditations such as mantram repetition and transcendental meditation may be really helpful for easing hyperarousal symptoms.”
Helping Veterans Find Calm
While there is still more research to be done, it’s becoming clearer that there are real benefits for veterans experiencing symptoms of PTSD through mindfulness activities. Veterans Outreach Center offers a weekly Meditation Monday group where veterans engage in somatic breathwork, which focuses on control and awareness of the breath to enhance overall well-being. Contact us today to learn more about our mindfulness and other health and wellness programs.